Table of Contents
If you’ve ever had red, itchy, or inflamed patches of skin that just won’t go away, you’re not alone. Many people experience skin rashes or reactions that are hard to explain. One cause of these rashes may be something called spongiotic dermatitis. This term might sound complicated, but we’re here to make it clear and easy to understand. Spongiotic dermatitis isn’t a disease itself—it’s a way doctors describe how your skin looks under a microscope when it’s irritated. It’s linked to many types of skin problems, including eczema, allergies, or contact with something that bothers your skin. In this friendly and helpful article, we’ll break down what spongiotic dermatitis really means, how it feels, what causes it, and what you can do to feel better. We’ll also share tips for avoiding flare-ups and answer the most common questions people ask about this skin condition. Let’s dive in and learn more about what your itchy skin might be trying to tell you.
What Is Spongiotic Dermatitis?
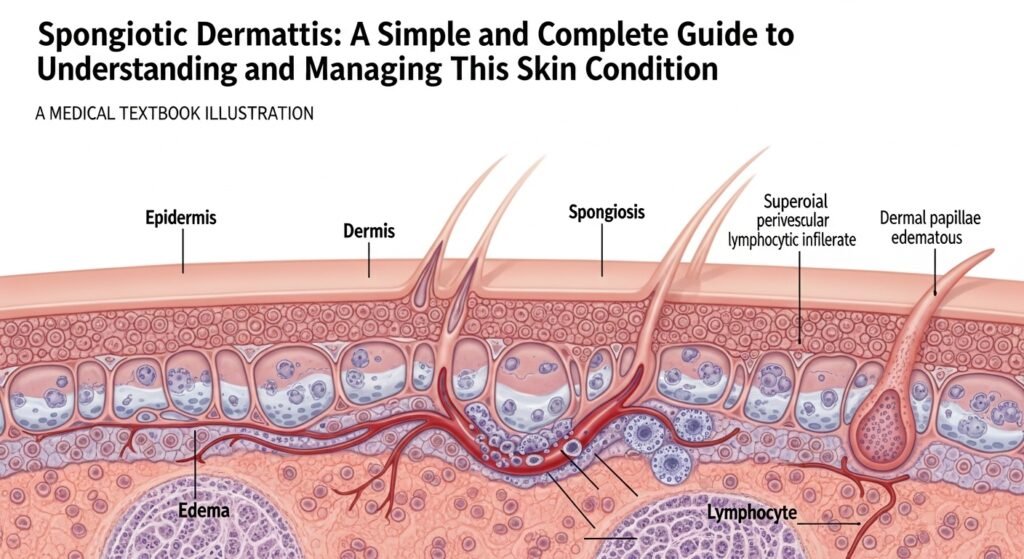
Spongiotic dermatitis is a medical term for swelling between the layers of your skin. It’s not a specific illness, but a sign that your skin is reacting to something—like an allergy, irritation, or immune response. The name comes from the word “spongiosis,” which means fluid builds up between skin cells, making them pull apart. When this happens, your skin may turn red, itchy, bumpy, or flaky. Doctors often discover spongiotic dermatitis during a skin biopsy, where a small piece of skin is examined under a microscope. In short, spongiotic dermatitis means your skin is inflamed, but the cause may vary.
Common Symptoms of Spongiotic Dermatitis
Everyone’s skin is different, but the signs of spongiotic dermatitis often look and feel similar. Some of the main symptoms include red patches, itchiness, dry or cracked skin, fluid-filled blisters, and skin that’s painful when touched. For some people, the rash is small and fades fast. For others, it may spread, become scaly, and leave dark or light spots after it heals. Common places on the body for these symptoms include your arms, legs, hands, chest, or neck. Sometimes the rash comes and goes. Other times, it may last for weeks or even longer.
What Causes Spongiotic Dermatitis?
There are many possible causes of spongiotic dermatitis, and most are linked to your body’s response to the outside world. Common triggers include contact with allergens (like poison ivy, soaps, or nickel), irritants (like cleaning products or fragrances), or even food allergies. Sometimes it’s caused by internal factors such as stress, a weak immune system, or genetics. It can also appear as a symptom of eczema, atopic dermatitis, or contact dermatitis. The skin is your body’s first line of defense, and when it reacts, inflammation can show up as spongiotic dermatitis.
Is Spongiotic Dermatitis the Same as Eczema?
Not exactly. Spongiotic dermatitis and eczema are related, but they’re not the same thing. Eczema is a condition that causes symptoms like dry, itchy, inflamed skin—and when a doctor takes a sample of that skin, it may show spongiosis under the microscope. That’s why eczema and spongiotic dermatitis often appear side by side. Think of eczema as what you feel and see on the outside, and spongiotic dermatitis as what’s going on inside your skin cells. Any kind of eczema—whether it’s contact, atopic, or dyshidrotic—can show signs of spongiosis.
How Is Spongiotic Dermatitis Diagnosed?
To diagnose spongiotic dermatitis, a dermatologist might start by asking about your medical history, your symptoms, and when the rash began. They’ll check your skin and ask about things like new soaps, pets, diet changes, or stress. Sometimes, a skin biopsy is needed. That means the doctor removes a tiny sample of the problem area, then studies it under a microscope. If they see spongiosis, they’ll know your skin is inflamed from either an allergic reaction, eczema, contact rash, or something similar. The biopsy helps them rule out other conditions like psoriasis, fungal infections, or skin cancer.
Treatment Options for Spongiotic Dermatitis
Good news! Most cases of spongiotic dermatitis can be treated with simple care. Once your doctor knows the cause, they may suggest treatments like topical corticosteroids, which help lower swelling and itching. You might also use moisturizing creams to protect your skin’s barrier and prevent dryness. For severe flare-ups, doctors might give oral antihistamines, antibiotics, or even light therapy. Avoiding whatever caused the reaction is a key part of healing. This could mean switching soaps, changing laundry detergent, or avoiding certain jewelry or metals. Treatment helps calm your current rash and prevent it from coming back.
Home Remedies to Help with Spongiotic Dermatitis
Along with doctor-approved treatments, many people find relief through gentle home remedies. Some helpful ideas include using cool compresses or oatmeal baths to soothe irritated areas. Moisturize twice a day with a thick, fragrance-free lotion. Try using natural oils like coconut or sunflower oil, which may help moisturize and heal the skin. Avoid hot showers, which can dry out your skin even more. Instead, bathe in lukewarm water and pat your skin dry gently. Choosing cotton clothes over wool or synthetic fabrics can also reduce itching and irritation.
Foods That May Trigger Symptoms
Some people notice that spongiotic dermatitis worsens after they eat certain foods. While not everyone has food-based reactions, common triggers include dairy, gluten, soy, eggs, nuts, and processed foods. These may cause inflammation in sensitive individuals. If you think food might be affecting your skin, try keeping a food diary to track what you eat alongside your symptoms. Share this with your doctor or an allergy specialist, who can help you decide whether an elimination diet might help. Remember, not every person with dermatitis has food triggers, but paying attention to your body’s response can be helpful.
How to Prevent Future Flare-Ups
Prevention is key when managing spongiotic dermatitis. Start by using gentle, fragrance-free products on your skin. Avoid allergens or irritants that caused past flare-ups. Maintain a consistent skincare routine that includes moisturizing often, especially after bathing. Wear gloves when cleaning or doing dishes. In dry weather, consider using a humidifier in your home. Reduce stress through light exercise, sleep, and mindfulness. Know your triggers—whether it’s detergent, jewelry, or even emotional stress—and work on avoiding or managing them. Following these steps can help reduce the number and severity of future breakouts.
When to See a Doctor
It’s time to call a doctor if your spongiotic dermatitis doesn’t get better after a few days of at-home treatment. If your rash gets worse, spreads quickly, oozes, or becomes very painful, it might be time for stronger medication or investigation into deeper causes. If you experience fever with the rash, seek care right away. Also, if flare-ups happen again and again, a dermatologist can help you find out what’s going wrong and help create a long-term treatment plan. Don’t suffer in silence—there’s help available, and you don’t have to deal with persistent flare-ups on your own.
How Long Does Spongiotic Dermatitis Last?
The length of a spongiotic dermatitis flare depends on what caused it and how it’s treated. Some mild cases clear up within a few days, while others may take weeks to show full healing. If you catch it early and start treating it fast, you may stop the inflammation before it spreads. Chronic or recurring cases—especially those linked to eczema—might flare up from time to time. In these situations, the goal is to keep symptoms under control and reduce how often flare-ups happen. Staying consistent with care and avoiding triggers goes a long way toward long-term relief.
FAQs
1. Is spongiotic dermatitis contagious?
No, it’s not contagious. You cannot catch it from anyone else, and it doesn’t spread from person to person.
2. Can stress cause spongiotic dermatitis?
Yes, stress is a known trigger. It can weaken your immune system and make flare-ups more likely.
3. What are the best creams for spongiotic dermatitis?
Fragrance-free moisturizers, corticosteroid creams, and barrier-protecting lotions are generally effective.
4. Does spongiotic dermatitis ever go away completely?
Some cases go away permanently, especially when the trigger is removed. Chronic types may need regular care.
5. Is spongiotic dermatitis the same as psoriasis?
No. While both are skin conditions, psoriasis is an autoimmune disease. Spongiotic dermatitis is more about allergic or irritant responses.
6. Should I stop all cosmetics if I have spongiotic dermatitis?
Not always. Start by avoiding scented or harsh products. Reintroduce one at a time after symptoms improve.
Final Thoughts
Spongiotic dermatitis may sound scary at first, but once you understand what it is and how to manage it, it becomes easier to live with. Whether it’s a one-time flare or a chronic part of your life, treating your skin with care and listening to what it’s telling you can make a big difference. Pay attention to signs, use gentle products, follow your doctor’s advice, and try not to stress—literally. Clearer, calmer skin takes time, but every small step helps. You’re not alone, and with the right guidance, you can feel better in your skin again.
